2022 AWARD WINNERS
Vicki Narron
- About
- Nomination Excerpts
Vicki graduated from nursing school in 1995 and, as she said, she has only ever worked at Duke University Hospital. As a CNIII, she is a Charge Nurse and Preceptor, in addition to caring for patients. With the onset of COVID and the expansion of the unit, Vicki advocated for the addition of a second Charge Nurse to focus on supporting new nurses. The new role would round to assist nurses with procedures they hadn’t performed before or to accompany them to take a patient off the unit to places they hadn’t been. Vicki proposed the idea to management, they approved, and the Patient Care Charge became a reality. The feedback about this new role has been amazing!
This nurse is one I aspire to be. She was my Preceptor as a Clinical Nurse I; she taught me how to precept; and she was my preceptor for the Charge Nurse role. She is the quintessential patient advocate, ALWAYS going above and beyond for her patient and their family. She also inspires integrity in others in her role as a leader for the MICU. I have learned so much from observing her and following in her footsteps.
Since the MICU became the designated COVID ICU for the hospital, she has been a true leader in helping us discover the best and safest ways to care for patients on isolation. She helped management to best organize how Charge Nurses should make the assignment based on isolation status and acuity, advocated for an increase in our nurse variable based on our increase in acuity and census, and worked with other nursing staff to innovate our pumps outside the room for isolation patients. She has also been a leader in our virtual staff meetings, speaking out as a strong voice for our Nursing and Respiratory Therapy staff, and conveying our needs for resources to upper management. I truly do not think we would have survived the pandemic without her support.
She spearheaded the Patient Care Charge (PCC) role for the MICU. In the height of COVID, the MICU was moved from a 24-bed unit to a 32-bed ICU in an attempt to expand our services and to be able to take on more patients. We were also in the midst of hiring and orienting many new nurses, the majority of them novice (Clinical Nurse I). She developed the idea for the role of the PCC to be more than just a resource nurse, but rather to focus on the new CNIs, with a focused role to round on them each shift, helping them with our Zero Harm Initiative; reviewing issues on our huddle board; answering questions about labs, care plans, etc. Our heightened acuity called for this role, as the majority of our patients were being proned and were on multiple drips, including paralytics. This role has also been instrumental as we are coming out of COVID, since the majority of our CNIs cared for mainly COVID patients while on orientation and did not get to experience our “usual” patient population. Since then, the PCC role has been focused on helping these new nurses understand liver failure, the special needs of oncology patients, the alcohol withdrawal pathway, etc.
This nurse has been a valuable leader for the unit during the transition between Nurse Managers. She has been an advocate for the nursing staff in communicating our needs to upper management (who is serving as our current Nurse Manager) and collaborating with new and experienced staff. She has also been a leader amongst our staff in being a loud voice for staff caring for the COVID population to be considered for appropriate incentives.
This nurse cares deeply for her patients and their families. I could provide so many examples, but one that comes to mind is a patient who had been the MICU for a long time with COVID-related Acute Respiratory Distress Syndrome (ARDS), and had many complications. She arranged for the family to be able to see the patient for a holiday by coordinating with the attending physician, the Charge Nurse that shift, and Respiratory Therapy. We mapped out a route to get the patient – in the hospital bed – moved out of the building so that the family could visit outside. The patient really needed this to lift spirits, and it was incredible to see the patient and family together, especially the patient’s toddler. This patient ended up spending a year in the hospital before being discharged. The nurse would go to visit the patient and family several times over the past year when the patient was on a stepdown unit.
This nurse exemplifies the true meaning of MICU nursing and is someone we should all aspire to be in our nursing practice.
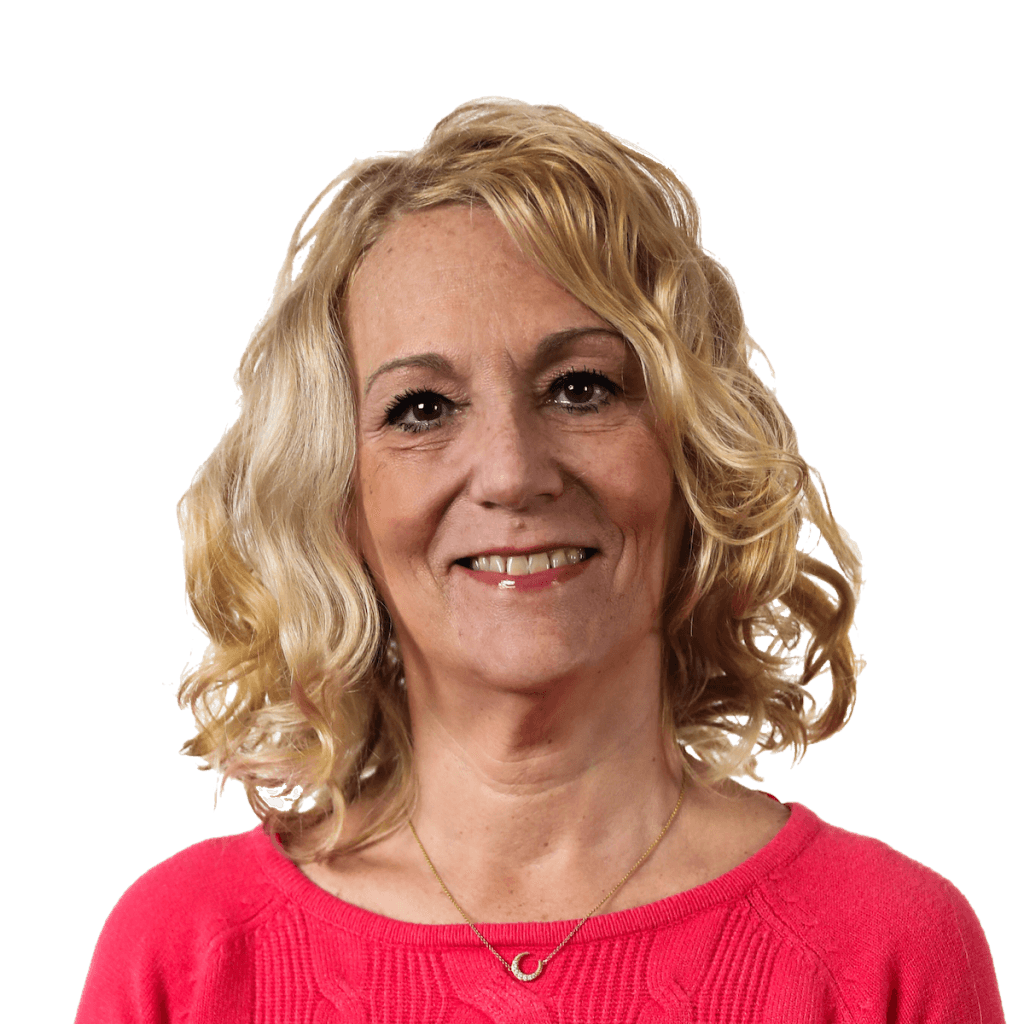
Vicki Narron
RN, CCRN
Clinical Nurse III
Medical Intensive Care Unit DMP 8 West
Duke University Hospital
Award: